

The ovaries are small, oval-shaped glands located on either side of your uterus. They produce and store your eggs (also called ovum) and make hormones that control your menstrual cycle and pregnancy. During ovulation, one of your ovaries releases an egg. If a sperm fertilizes this egg, you can become pregnant. Your ovaries continue to release an egg each menstrual cycle until you reach menopause. During menopause, your ovaries stop releasing eggs. Sometimes your ovaries can release more than one egg (this can result in a multiple pregnancy). You are born with all the eggs you will ever have in your lifetime. Your ovaries play a critical role in both menstruation and conception. They produce eggs for fertilization and they make the hormones estrogen and progesterone. An ovary releases an egg around the middle of your menstrual cycle (around day 14 of a 28-day cycle) in a process called ovulation. Each of your ovaries has thousands of ovarian follicles. Ovarian follicles are small sacs in the ovaries that hold immature eggs. Each month, between days six and 14 of your menstrual cycle, follicle-stimulating hormone (FSH) causes follicles in one of your ovaries to mature. At about day 14 in the menstrual cycle, a sudden surge in luteinizing hormone (LH) causes the ovary to release an egg (ovulation). The egg begins its travel through a narrow, hollow structure called the fallopian tube to the uterus. As the egg travels through the fallopian tube, the level of progesterone rises, which helps prepare the uterine lining for pregnancy. If you don't become pregnant that cycle, the egg disintegrates and gets reabsorbed by your body so menstruation can begin. Your ovaries secrete estrogen and progesterone. These hormones play an important role in reproductive development and menstruation. Estrogen production is highest in the first half of your menstrual cycle before ovulation. Progesterone rises during the second half of your cycle to prepare your uterus for a fertilized egg (if conception occurs). Ovaries are the female gonads — the primary female reproductive organs. These glands have three important functions: they secrete hormones, they protect the eggs a female is born with and they release eggs for possible fertilization.
Ovaries are the female gonads — the primary female reproductive organs. These glands have three important functions: they secrete hormones, they protect the eggs a female is born with and they release eggs for possible fertilization.
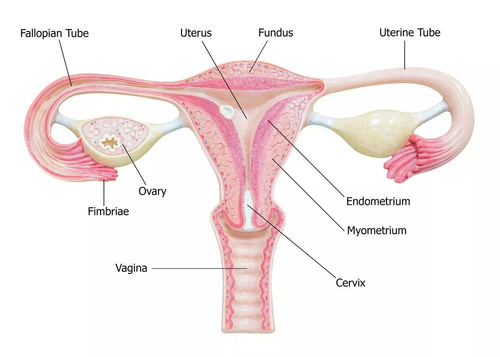
Human females are typically born with two ovaries stemming from the uterus. Before puberty, ovaries are just long bundles of tissue. As the female matures, so do her ovaries. When mature, ovaries are about the size of a large grape, according to EndocrineWeb. The ovaries lie on either side of the uterus against the pelvic wall in a region called the ovarian fossa.
They are held in place by ligaments attached to the uterus. The ovaries have three functions. First, they shelter and protect the eggs a female is born with until they are ready for use. It is thought that women are born with their lifetime supply of eggs, but a study by the University of Edinburgh's School of Biological Sciences found that chemotherapy might spark the development of new eggs.
Unilateral ovarian absence (UOA) is a rare event. It has a prevalence of one in 11,240 women. Even rarer is the absence of both the ovary and distal portion of the ipsilateral fallopian tube. It has been suggested that this phenomenon may be a result of a congenital malformation or an ischemic event due to mechanical alterations. torsion and subsequent resorption of the ovary) that occur during fetal life or childhood.
Sex hormone release by the ovary is dependent on the phase of the menstrual cycle. During the first phase of the cycle, the follicular phase, the follicles are developing. Finally, the dominant follicle will turn into a preovulatory follicle, starting to release estrogens as it continues its maturation process. After ovulation, during the luteal phase of the menstrual cycle, preovulatory follicles turn into the corpus luteum, which releases progesterone. On the other hand, antral and preantral follicles that form the ovarian reserve produce a hormone called Anti-Müllerian hormone throughout the entire cycle, regardless of the phase.
Folliculogenesis is the process in which a recruited primordial follicle grows and develops into a specialized graafian follicle with the potential to either ovulate its egg into the oviduct at mid-cycle to be fertilized or to die by atresia. In women, the process is long, requiring almost 1 year for a primordial follicle to grow and develop to the ovulatory stage. During the course of folliculogenesis, growth is achieved by cell proliferation and formation of follicular fluid, whereas development involves cytodifferentiation of all the cells and tissues in the follicle. Only a few follicles in the human ovary survive to complete the cytodifferentiation process, with 99.9% dying by a programmed cell death mechanism called apoptosis.
The mechanisms regulating follicle growth and development are under the control of changing concentrations of ligands (i.e. hormones and growth factors). At the endocrine level, folliculogenesis is regulated by a central nervous system, anterior pituitary, and ovary cascade mechanism. Specialized hypothalamic neurons secrete pulses of gonadotropin-releasing hormone (GnRH) into the portal blood vessels, which acts on the gonadotrophs to cause a pulsatile release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which act on ovarian follicle cells to control folliculogenesis. Although GnRH, FSH, and LH are critically important in regulating folliculogenesis, hormones and growth factors, which are themselves products of the follicle, can act locally to modulate (amplify or attenuate) FSH and LH action. This is the autocrine/paracrine system of developing follicles. It is believed that this local regulatory system plays an important role in the complex mechanisms governing the timing of folliculogenesis and whether a follicle becomes dominant or atretic.
The first major event in folliculogenesis is recruitment. Recruitment is the process by which an arrested primordial follicle is triggered to reinitiate development and enter the pool of growing follicles. All primordial follicles (oocytes) present in the human ovaries are formed in the fetus between the sixth and the ninth month of gestation. Because the entire stock of oocytes in primordial follicles is in meiotic prophase, none is capable of dividing mitotically. All oocytes (primordial follicles) capable of participating in reproduction during a woman's life are present in the ovaries at birth. The total number of primordial follicles in the ovaries at any given moment of time is called the ovary reserve (OR).7 The process of recruitment begins soon after the formation of the primordial follicles in the fetus,8 and it continues throughout the life of the female until the pool of primordial follicles is exhausted at the menopause. There is a bi-exponential decrease in OR during aging 7,9,10. The number of primordial follicles falls steadily for more than three decades, but when the OR reaches a critical number of about 25,000 at 37.5 ± 1.2 years of age, the rate of loss of primordial follicles accelerates about twofold. This change in OR is associated in an age-related decrease in fecundity, perhaps causal to the age-related increase in FSH that occurs in women after 36 years of age.
Diminished ovarian reserve is when you have fewer eggs in your ovaries compared to people your age. It’s sometimes called low egg count or low ovarian reserve. Your eggs are the building blocks (along with sperm) for pregnancy. Your egg count will decrease as you age, but this happens sooner than expected for some people. Diminished ovarian reserve makes it harder to get pregnant. Your healthcare provider diagnoses low ovarian reserve with ovarian reserve testing. Just because you have diminished ovarian reserve doesn't mean you can't get pregnant. It means you may find getting pregnant more difficult or need to consider fertility treatment
Women or people assigned female at birth (AFAB) are born with all the eggs they’ll ever produce. Your age is the strongest predictor of egg supply. Studies show that the rate of egg loss increases once you turn 35.
Actual numbers vary from person to person, but these are the average number of
eggs you have throughout life:
* Birth: 1 to 2 million eggs.
* Puberty: 300,000 to 400,000 eggs.
* Age 40: 25,000 eggs.
* Menopause: less than 1,000 eggs.
Most people don’t have symptoms other than not getting pregnant after months or years of regular sexual intercourse. Others may notice their menstrual cycle getting consistently shorter.
If you’re experiencing symptoms of primary ovarian insufficiency, you may have symptoms of perimenopause such as:
* Hot flashes.
* Irregular menstrual periods.
* Vaginal dryness.
Aging is one of the biggest causes of low ovarian reserve; however, sometimes, there is no cause. Other times, genetics or medical treatments cause diminished ovarian reserve. These include:
* Genetic disorders that affect the X chromosome.
* Radiation or chemotherapy (cancer treatment).
* Having surgery on your ovaries.
* Losing one or both of your ovaries.
* Autoimmune conditions.
There is no way to reverse diminished ovarian reserve or produce more eggs. Once your healthcare provider suspects that you have low ovarian reserve, they’ll work with you on a treatment plan that helps you reach your pregnancy goals. This treatment plan will be determined by how soon you would like to get pregnant, how many children you would like to have, finances and the strength of your desire to have a child who is genetically related to you. Treatment options may include freezing your eggs for later use, attempting to conceive naturally or undergoing IVF with your own eggs .
Freezing your eggs is one way to preserve your fertility. If your provider says you are at high risk for low ovarian reserve, they may suggest freezing your eggs before your egg count declines further. Egg freezing involves taking hormones to stimulate your ovaries to make as many eggs as possible. Then, the mature eggs are collected and frozen for future IVF treatment. In some cases, your provider will suggest creating embryos, meaning that they would fertilize the mature eggs with your partner’s sperm before freezing them for future use or transferring them to your uterus to get pregnant.
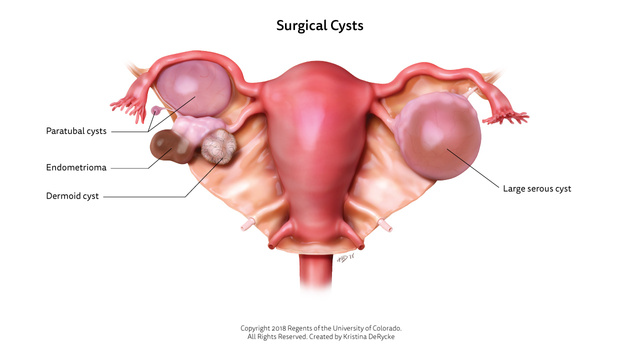
An ovarian endometrioma is a cyst that’s filled with the same fluid that’s in the lining of your uterus (endometrium). Sometimes called “chocolate cysts,” the fluid inside an ovarian endometrioma resembles chocolate syrup. Instead of being in your uterus, though, ovarian endometriomas form in your ovaries. Having an ovarian endometrioma is a sign that you have endometriosis, a condition that happens when endometrioal-like tissue take hold in places outside your uterus.
Anyone who menstruates can get endometriosis. And only people with endometriosis get ovarian endometriomas. You’re more likely to have endometriosis if you’re between ages 25 and 40. The American Society for Reproductive Medicine (ASRM) has identified four different stages of endometriosis. What stage you’re in depends on how much endometrial-like tissue is outside your uterus, its characteristics, and how deeply it’s embedded in the organ where it’s found, like an ovary. If you have an ovarian endometrioma, you’re in Stage 3 or 4.
Stage 1:
You have a small amount of tissue, mostly surface-level on the organ where it’s found.
Stage 2:
You have more tissue than in Stage 1, and some of it is embedded.
Stage 3:
You have a lot of tissue that’s deeply embedded, including small endometriomas.
Stage 4:
You have a lot of tissue that’s deeply embedded, including large endometriomas.
About 10% of people who menstruate have endometriosis, and about 17 to 44% of those with endometriosis are estimated to have ovarian endometriomas.
Doctors don’t know for sure what causes endometriosis or ovarian endometriomas. The most common theory is that endometriosis happens because some of the endometrial-like tissue that you shed when you menstruate flows backward (retrograde menstruation). Instead of leaving your body through your vagina, some of the tissue travels back through your fallopian tubes and into your ovaries. Each menstrual cycle when your body releases the hormones that make your uterus lining bleed, the out-of-place tissue bleeds, too. It becomes inflamed. Over time, the menstrual blood and the inflamed tissue around it can become an ovarian endometrioma.
Pain or tenderness in your pelvis is the most common way to know that you have an ovarian endometrioma. You may notice other symptoms, too:
* Periods that are especially painful.
* Pain during intercourse (dyspareunia).
* Pain when you’re peeing or pooping.
* Feeling the urge to pee more.
* Back pain.
* Vomiting.
* Bloating.
* Nausea.
There isn’t a cure for ovarian endometriomas, but your provider can remove them if they cause unpleasant symptoms or pose risks to your health.
* Monitoring:
You and your provider may choose to monitor your cysts if they’re small and not causing symptoms.
* Laparoscopy:
Your provider may recommend a laparoscopy if you have ovarian endometriomas that are painful, growing or bigger than 4 centimeters. The risks increase that the cyst will become cancerous once it reaches this size. Removing the cyst not only helps improve your symptoms but it also reduces the risk that there’ll be continued damage to ovarian tissue, like having an ovarian endometrioma burst. It may improve your chances of becoming pregnant if you’ve had fertility issues because of ovarian endometriomas.
* Hysterectomy/Oophorectomy:
you don’t have plans to become pregnant, your provider may recommend that you have your uterus (hysterectomy) and/or ovaries (oophorectomy) removed. The best treatment for you depends on lots of factors, like your age, your risk for cancer, your plans for becoming pregnant, including whether or not you’re thinking of in vitro fertilization (IVF). Your provider can recommend the best treatment options based on your unique situation More research is needed to understand how laparoscopy affects fertility in couples who are trying to become pregnant through IVF. Some research suggests that this procedure can reduce the amount of eggs the ovary makes that are capable of being fertilized (ovarian reserve). This can make it harder to become pregnant. If your ovarian endometriomas are making it hard for your provider to access and collect your eggs, it may be a good idea to remove the ovarian endometriomas regardless.
Weigh the pros and cons of removing your ovarian endometriomas with your provider to decide the best plan for your family planning goals and your health
The female genital tract may be affected by ascending infection, either from sexually transmitted infections or vaginal flora, or occasionally from secondary infections from gastrointestinal sources. Pelvic inflammatory disease (PID) refers to acute and subclinical infection of the upper genital tract, involving any or all of the uterus, fallopian tubes, and ovaries; this is often accompanied by involvement of the neighboring pelvic organs. It results in endometritis, salpingitis, oophoritis, peritonitis, perihepatitis, and/or tubo-ovarian abscess (TOA).
A complication of PID may be a TOA, which is an inflammatory mass involving the fallopian tube, ovary, and, occasionally, other adjacent pelvic organs. This may manifest as a tubo-ovarian complex (an agglutination of those structures) or a collection of pus (TOA). These abscesses are found most commonly in reproductive-age patients and typically result from upper genital tract infection. TOA typically occurs as a complication of PID.
A TOA or complex is a serious and potentially life-threatening condition. Aggressive medical and/or surgical therapy is required, and rupture of an abscess may result in sepsis. The mortality rate associated with TOA was approximately 50 percent or higher prior to the advent of broad-spectrum antibiotics and modern surgical practice. In current practice, the mortality rate approaches zero for abscesses that have not ruptured. Current mortality rates for patients with ruptured abscesses are not reported in the literature; data from the 1960s suggested a mortality rate ranging from 1.7 to 3.7 percent.
A woman with a TOA may feel a mass in their lower abdomen or pelvis. They may also have symptoms of an infection, which includeTrusted
* chills
* fever
* nausea
* pain or tenderness in the lower abdomen
* vaginal bleeding
* unusual and heavy vaginal discharge
After examining and testing a person, a doctor may find the following symptoms of a TOA: pus-filled ovaries
cervical excitation, or tenderness when a doctor moves the cervix with their gloved hand elevated levels of white blood cells
PID-causing pathogens present in the cervix or vagina can travel up to the endometrium and ascend through the fallopian tubes into the peritoneal cavity, where they form a mass. Most cases of a TOA are associated with peritonitis — inflammation of the peritoneal cavity lining.
According to a 2018 study published in the International Journal of Obstetrics and GynecologyTrusted Source, a TOA is usually polymicrobial in 30–40% of cases. This means multiple pathogens such as bacteria or fungi may be present.
Researchers have identified some microorganisms in TOA cases. They include:
* Escherichia coli (E. coli)
* Bacteroides fragilis (B. fragilis)
* Peptostreptococcus anaerobius
* aerobic Streptococci
* Neisseria gonorrhea (N. gonorrhea)
* Chlamydia trachomatis (C. trachomatis)
Infections from adjacent organs, such as the appendix, may spread and cause a TOA. The blood can also carry infections from elsewhere in the body.
A TOA may also arise when cancer invades healthy cells of the female reproductive system and spreads to surrounding tissues.
Xanthogranulomatous inflammation
Antibiotic medication
This is usually the first-line treatment for people with a TOA. A doctor may prescribe the following dosages of broad-spectrum antibiotics: 1 milligram (mg) of intramuscular ceftriaxone plus 100 mg of oral doxycycline administered twice daily 900 mg intravenous (IV) clindamycin administered every 8 hours with 5 mg per kilogram of body weight IV gentamicin
Alternative:
3 grams of ampicillin/sulbactam administered every 6 hours with 100 mg oral dosages of doxycycline administered twice daily A doctor will administer fluids and medications in the first 24 hours following the diagnosis of a TOA. They will observe a person’s vital signs until symptoms improve significantly. If antibiotic therapy is effective, a patient may spend 3–4 days in the hospital. Research from 2020 suggests that antibiotic therapy is effective in 70% of cases.
Doctors may recommendTrusted Source surgery for a TOA in the following circumstances * an abscess that is too large * ineffective antibiotic therapy * rupture of the TOA Surgery aims to drain the abscess, remove the affected parts, and prevent further damage. This includes:
Laparoscopy:
This minimally invasive surgery allows doctors to drain any abscess and remove damaged tissues in the female reproductive system.
Salpingectomy:
If there is damage to the fallopian tube, the doctor will perform a salpingectomy to remove it and prevent further infection.
Oophorectomy:
Following a TOA rupture, a doctor will remove a damaged ovary by performing an oophorectomy.
Taking care of yourself at home
* get plenty of rest
* avoid lifting heavy weights
* eat a balanced diet
* drink enough water
* avoid sexual intercourse for at least 6 weeks
* wear loose clothing
* clean the incision site following the doctor’s instructions
* take medications according to the prescription
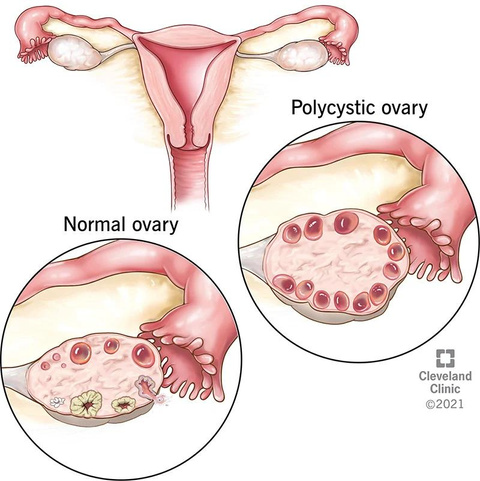
PCOS is a problem with hormones that affects women during their childbearing years (ages 15 to 44).
Between 2.2 and 26.7 percent of women in this age group have PCOS. Many women have PCOS but don’t know it. In one study, up to 70 percent of women with PCOS hadn’t been diagnosed . PCOS affects a woman’s ovaries, the reproductive organs that produce estrogen and progesterone — hormones that regulate the menstrual cycle. The ovaries also produce a small amount of male hormones called androgens. The ovaries release eggs to be fertilized by a man’s sperm. The release of an egg each month is called ovulation. Follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are produced in the pituitary gland, control ovulation. FSH stimulates the ovary to produce a follicle — a sac that contains an egg — and then LH triggers the ovary to release a mature egg. PCOS is a “syndrome,” or group of symptoms that affects the ovaries and ovulation. Its three main features are:
* cysts in the ovaries
* high levels of male hormones
* irregular or skipped periods
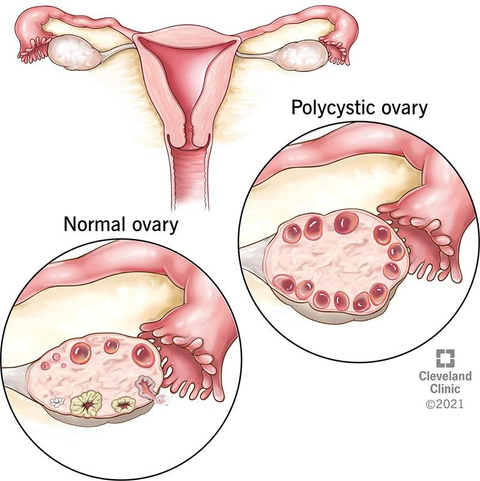
In PCOS, many small, fluid-filled sacs grow inside the ovaries. The word “polycystic” means “many cysts.” These sacs are actually follicles, each one containing an immature egg. The eggs never mature enough to trigger ovulatio The lack of ovulation alters levels of estrogen, progesterone, FSH, and LH. Progesterone levels are lower than usual, while androgen levels are higher than usua Extra male hormones disrupt the menstrual cycle, so women with PCOS get fewer periods than usua PCOS isn’t a new condition. Italian physician Antonio Vallisneri first described its symptoms in 1721
Doctors don’t know exactly what causes PCOS. They believe that high levels of male hormones prevent the ovaries from producing hormones and making eggs normally. Genes, insulin resistance, and inflammation have all been linked to excess androgen production.
Studies show that PCOS runs in families.
It’s likely that many genes — not just one — contribute to the condition.
Up to 70 percent of women with PCOS have insulin resistance, meaning that their cells can’t use insulin properly . Insulin is a hormone the pancreas produces to help the body use sugar from foods for energy. When cells can’t use insulin properly, the body’s demand for insulin increases. The pancreas makes more insulin to compensate. Extra insulin triggers the ovaries to produce more male hormones. Obesity is a major cause of insulin resistance. Both obesity and insulin resistance can increase your risk for type 2 diabetes . Inflammation Women with PCOS often have increased levels of inflammation in their body. Being overweight can also contribute to inflammation. Studies have linked excess inflammation to higher androgen levels .
Some women start seeing symptoms around the time of their first period. Others only discover they have PCOS after they’ve gained a lot of weight or they’ve had trouble getting pregnant. The most common PCOS symptoms are: * Irregular periods. A lack of ovulation prevents the uterine lining from shedding every month. Some women with PCOS get fewer than eight periods a year or none at all (10Trusted Source). * Heavy bleeding. The uterine lining builds up for a longer period of time, so the periods you do get can be heavier than normal. * Hair growth. More than 70 percent of women with this condition grow hair on their face and body — including on their back, belly, and chest (11). Excess hair growth is called hirsutism. * Acne. Male hormones can make the skin oilier than usual and cause breakouts on areas like the face, chest, and upper back. * Weight gain. Up to 80 percent of women with PCOS are overweight or have obesity (11). * Male pattern baldness. Hair on the scalp gets thinner and may fall out. * Darkening of the skin. Dark patches of skin can form in body creases like those on the neck, in the groin, and under the breasts. * Headaches. Hormone changes can trigger headaches in some women.
Treatment for PCOS usually starts with lifestyle changes like weight loss, diet, and exercise. Losing just 5 to 10 percent of your body weight can help regulate your menstrual cycle and improve PCOS symptoms (11, 20Trusted Source). Weight loss can also: * improve cholesterol levels * lower insulin * reduce heart disease and diabetes risks Any diet that helps you lose weight can help your condition. However, some diets may have advantages over others. Studies comparing diets for PCOS have found that low carbohydrate diets are effective for both weight loss and lowering insulin levels. A low glycemic index (low GI) diet that gets most carbohydrates from fruits, vegetables, and whole grains helps regulate the menstrual cycle better than a regular weight loss diet. A few studies have found that 30 minutes of moderate-intensity exercise at least 3 days a week can help women with PCOS lose weight. Losing weight with exercise also improves ovulation and insulin levels. Exercise is even more beneficial when combined with a healthy diet. Diet plus exercise helps you lose more weight than either intervention alone, and it lowers your risks for diabetes and heart disease. There is some evidence that acupuncture can help with improving PCOS, but more research is needed.
Primary ovarian insufficiency (POI) is a condition that occurs when a person’s ovaries fail earlier than average. Your ovaries are small glands located on both sides of your uterus that produce and release eggs during ovulation. Your ovaries also make important hormones for menstruation, pregnancy and other bodily functions. The usual age for egg production to stop, known as menopause, is around 51. For some people, POI happens abruptly, and they suddenly stop having a regular menstrual period. But, for others, a diagnosis of POI comes after months or years of irregular periods. Primary ovarian insufficiency was previously known as premature ovarian failure. However, healthcare providers prefer “insufficiency” rather than “failure” because research has shown that people with POI can have intermittent ovulation. This means you may still release an egg and get pregnant if you have POI. In fact, around 5% to 10% of those with a diagnosis of POI will spontaneously get pregnant without treatment for infertility. For this reason, POI is often also called “decreased ovarian reserve.”
In the majority of cases, healthcare providers don’t know what causes primary ovarian insufficiency (idiopathic POI). However, research shows that up to one-third of cases may have a hereditary component. Some other causes of POI include: * Autoimmune disorders like Addison disease, rheumatoid arthritis or thyroid disease. * Cancer treatments such as chemotherapy and radiation. * Genetic disorders including Turner syndrome (genetic disorder involving an abnormality in one of a person AFAB’s two X chromosomes) or Fragile X syndrome (a genetic disorder involving changes in the gene FMR1). * Hysterectomy (surgery to remove your uterus). * Infections like mumps and HIV. (This is thought to happen due to antibodies that attack your ovary.) * Prolonged exposure to chemicals, pesticides, cigarette smoke and other toxins.
The most common sign of POI is irregular or missed periods. Some people with primary ovarian insufficiency don’t have any noticeable symptoms. Other symptoms can include: * Irregular or missed periods. * Trouble getting pregnant. * Decreased sex drive. * Difficulty concentrating. * Irritability. * Dry eyes. * Hot flashes and night sweats. * Vaginal dryness. * Painful sex due to vaginal dryness
Doctor will perform a physical exam and a pelvic exam. They’ll also ask you about your health history. Knowing about your typical menstrual cycle, previous pregnancies or use of birth control is helpful to your provider in diagnosing POI. Next, they will likely order blood tests to measure levels of certain hormones in your body. These include follicle stimulating hormone (FSH), estrogen and prolactin. Other tests your provider may use include: * A blood test (karyotype testing) to look for genetic disorders. * A pelvic ultrasound (to look at your ovaries and uterus). * A pregnancy test. * Antibody tests to check for autoimmune disorders
We providers treat POI in different ways. It depends on your age, symptoms and if you wish to get pregnant. Primary ovarian insufficiency treatment involves: * Replacing hormones that your ovaries no longer produce. * Treating symptoms or side effects of POI (like night sweats, vaginal dryness, etc.). * Lowering your risk for conditions that POI causes. * Treating underlying conditions that worsen POI symptoms.
Hormone therapy gives your body the hormones that your ovaries aren’t making. Hormone therapy may involve taking just estrogen or taking estrogen and progesterone. Hormone therapy can help reduce symptoms of POI like night sweats and vaginal dryness. It will also lower your risk for osteoporosis and other conditions that POI can cause. Your provider may prescribe hormone therapy in different ways, such as a pill, cream, gel, patch or vaginal ring. If you begin HRT, you’ll continue treatment up until the age when natural menopause typically begins (age 51 to 52). Discuss the benefits and risks of HRT with your provider to make sure it’s right for you. In addition to HRT, other treatments could include: * Taking calcium and vitamin D to help lower your risk of osteoporosis. * Getting regular physical exercise, lifting weights (for your bone health) and maintaining a healthy weight. * Exploring options for fertility treatment if you wish to expand your family.
Ovarian hyperstimulation syndrome (OHSS) occurs when a woman’s ovaries swell and leak fluid into the body. This condition is a complication that can occur in women who receive fertility treatments that stimulate the ovaries to produce more eggs than usual, but there are rare cases of OHSS occurring spontaneously. In the past, OHSS was a relatively common complication of in vitro fertilization (IVF). New protocols and strategies have made this condition rare, except for mild cases. OHSS is more common in women receiving fertility treatments who have polycystic ovarian syndrome (PCOS). PCOS is a reproductive disorder involving a hormonal imbalance. Most cases of OHSS are mild and cause temporary discomfort. Severe cases of the condition are rare but can be life-threatening.
In most cases, OHSS develops because of high levels of the pregnancy hormone hCG following fertility treatments that stimulate the production of many eggs at one time, as is done with many IVF protocols. In very rare cases, patients have genetic mutations in certain hormone receptors that predispose them to developing OHSS even without hormonal treatments. In women with OHSS, drugs used in fertility treatments cause the blood vessels surrounding the ovaries to leak fluid. This fluid causes the ovaries to swell. Sometimes this fluid moves into the belly and other areas, causing: * Swelling. * Pain. * Nausea. * Vomiting. * Increased thirst.
The signs and symptoms of OHSS vary depending on the severity of the condition. Symptoms of mild to moderate OHSS include: * Abdominal pain. * Bloating. * Sleight weight gain. * Nausea. * Sometimes other symptoms like: * Excessive weight gain. * Severe nausea and vomiting. * Severe abdominal swelling. * Difficulty breathing. * Blood clots. * Decreased urination. * Kidney failure. * Severe abdominal pain.
Doctors diagnose OHSS with several tests. These tests can include:
Checks your weight and measures the size of your waist to look for signs of swelling.
Looks for free fluid in the abdomen and the size of the ovaries.
Looks for fluid in the chest.
Measures hormone levels for signs of OHSS.
The treatment for OHSS varies depending on how severe the condition is. Treatment aims to manage symptoms and avoid complications. For mild to moderate cases of OHSS, treatment usually involves: * Avoiding vigorous physical activity. * Increasing oral intake of fluids. * Using acetaminophen to relieve symptoms. * Weighing yourself daily. * Monitoring yourself for any severe symptoms. * Severe cases of OHSS often require hospitalization. Treatment of severe OHSS may include: * Adjusting your fertility medication dose. * Receiving intravenous (directly into the vein) fluids. * Freezing your embryos and delaying their embryo transfer until the ovaries return to normal. * Undergoing paracentesis (a procedure to remove fluid from the belly). * Taking medicines to ease symptoms or reduce activity in the ovaries.
Ovarian stimulation is a treatment used before other assisted conception procedures to both induce ovulation and to increase the number of eggs released. This can increase the chances of a pregnancy happening. Ovarian stimulation can be done either with medications, or it can be done using injections. Ovarian insemination may precede artificial insemination or in vitro fertilisation (IVF). Ovarian stimulation is performed to increase the number of eggs released in ovulation. If done before artificial insemination, this increases the chances of the inseminated sperm of reaching the fallopian tube and fertilising an egg. It is done before IVF so that more than one egg is retrieved during egg retrieval. This allows more than one egg to be mixed with semen in a laboratory setting to increase the chances of a viable embryo forming for transferring.
The treatment consists of putting an injection of follicle stimulating hormone (FSH) and/or luteinising hormone (LH), given usually 8-10 days after the end of the last period. The goal is to help the ovaries produce one or more eggs for release. Ovarian stimulation may also consist of taking medication orally instead. Once ovulation occurs and one or more eggs are released, either egg retrieval for IVF can take place, or artificial insemination can be carried out.
Ovarian cancer occurs when abnormal cells in your ovaries or fallopian tubes grow and multiply out of control. Ovaries are part of the female reproductive system. These two round, walnut-sized organs make eggs during your reproductive years. Ovarian cancer affects women and people assigned female at birth (AFAB). It’s slightly more common in Native American and white populations than in people who are Black, Hispanic or Asian. In addition, people of Ashkenazi Jewish descent are much more likely to have a BRCA gene mutation, placing them at a higher risk for breast and ovarian cancer. Ovarian cancer accounts for 1% of all new cancer cases in the U.S. The lifetime risk of developing ovarian cancer is approximately 1 in 78.
Stage I: This stage is divided into three sub-stages (Stage IA, Stage IB and Stage IC). In the first substage, cancer is only in one ovary or one fallopian tube. Stage IB has cancer in both ovaries or fallopian tubes. In Stage IC, cancer is in both ovaries or fallopian tubes and is found outside of your ovary (on the outside of the organ itself or in the space around the ovary, called the peritoneal cavity). Stage II: Stage II is also divided into a few additional stages. In Stage IIA, the cancer is no longer only in your ovary, but has also spread to your uterus. In Stage IIB, the cancer has spread to other nearby structures in your pelvis. Stage III: This stage includes three sub-stages. In Stage IIIA, the cancer has spread beyond your pelvis to your abdomen (microscopically) or within lymph nodes. The second sub-stage (Stage IIIB), the tumor is up to 2 centimeters in size and has spread beyond your pelvis or within your lymph nodes. In Stage IIIC, the cancer has moved outside of your pelvis area and is larger in size (more than 2 centimeters) or may be within your lymph nodes. At this point, it could impact other organs, like your liver and spleen. Stage IV: Stage IV cancer is the most severe. In this stage, the cancer has spread to the inside of organs such as your liver or spleen. In Stage IVA, it’s found near your lungs, and in Stage IVB, the cancer has spread to the lymph nodes of your groin or into your chest.
The exact cause of ovarian cancer isn’t yet known. But some people have a slightly higher risk of developing the condition. Ovarian cancer risk factors include: Being over the age of 60. Obesity. A family history of ovarian cancer (others in your biological family have had the disease) or have inherited a gene mutation (BRCA1 or BRCA2) or Lynch syndrome. Never being pregnant or having children later in life. Endometriosis.
Ovarian cancer can develop and spread throughout your abdomen before it causes any symptoms. This can make early detection difficult. Ovarian cancer symptoms may include: Pelvic or abdominal pain, discomfort or bloating. Changes in your eating habits, getting full early and losing your appetite. Vaginal discharge or abnormal bleeding, especially if the bleeding occurs outside of your typical menstrual cycle or after you’ve gone through menopause. Bowel changes, such as diarrhea or constipation. An increase in the size of your abdomen. Peeing more often (frequent urination).
The goal in treating cancer is to remove as much, if not all, cancer from your body as possible. Common ovarian cancer treatments include: Surgery. This typically involves the removal of your reproductive organs and any organ that has cancer on it. Your surgeon may use laparoscopy (a minimally invasive surgery) or laparotomy (open surgery that requires an abdominal incision). Chemotherapy. Your provider may recommend chemotherapy either before or after surgery. Chemotherapy are drugs designed to target and kill cancerous cells. Your provider may give you chemotherapy intravenously (through a vein) or orally (in pill form). Targeted therapy. This cancer treatment uses drugs to identify and attack cancer cells. Targeted therapy changes the way cancer cells grow and divide. Hormone therapy. Some ovarian cancers use hormones to grow. This type of therapy blocks hormones, slowing or stopping the growth of cancer. Radiation therapy. Providers rarely use radiation therapy for treatment of ovarian cancer. After you’ve completed ovarian cancer treatment, your healthcare provider will want to see you regularly for observation. You may have routine appointments to check and make sure the cancer hasn’t returned over time. During these appointments, your provider may go through any possible symptoms and do an exam. Be mindful of any symptoms you may be having and tell your provider about them. Sometimes, your provider may order imaging tests, typically a CT scan.
An adhesion is a band of scar tissue that joins two internal body surfaces that are not usually connected. Organs or tissues within the body stick (adhere) to other internal surfaces. Adhesions develop as the body attempts to repair itself. This normal response can occur after surgery, infection, injury (trauma) or radiation. Adhesions may appear as thin sheets of tissue similar to plastic wrap, or as thick fibrous bands. Adhesions can affect the female reproductive organs (ovaries, fallopian tubes), the bowel, the area around the heart, the spine and the hand. They can cause a range of problems including infertility, dyspareunia (painful intercourse), pelvic pain and bowel obstruction or blockage. Adhesions can also lead to a complex set of problems called adhesion-related disorder (ARD). Adhesions are a widespread problem. Up to 93 per cent of people who have abdominal surgery go on to develop adhesions. Abdominal adhesions also occur in 10 per cent of people who have never had surgery
Although adhesions can affect endometriosis symptoms, an adhesion comes with its own set of separate symptoms. That’s why your symptoms might change when you develop endometriosis adhesions. Adhesions may cause: chronic bloating cramping nausea constipation loose stools pain that changes with position or stretching
Adhesion removal carries a risk of the adhesion coming back or causing more adhesions. It’s important to be mindful of this risk when you consider having an endometriosis adhesion removed. Adhesions are removed through a type of surgery called adhesiolysis. The location of your adhesion will determine what kind of surgical treatment is best for you. For example, laparoscopic surgery is less invasive and can break up and remove an adhesion that blocks your bowels. Laparoscopic surgery is also less likely to create more adhesions during the healing process. More research about the outcomes of adhesion removal is needed. The success rate appears connected to area of your body where the adhesion is. Surgeries for adhesions to the bowel and abdominal wall tend to have a lower rateTrusted Source of adhesions returning after surgery compared to other organs.
When you have an endometriosis adhesion, finding a way to manage your symptoms can be a process. Different things work for different people. Over-the-counter pain medications, such as ibuprofen (Advil) and acetaminophen (Tylenol), can help minimize the pain, but they sometimes aren’t enough. Sitting in a warm bath or reclining with a hot water bottle when your pain flares up can help relax your muscles and soothe the pain from the adhesion. Your doctor may also recommend massage techniques and physical therapy to try to break up the scar tissue and lessen the pain. This condition can impact your sex life, your social life, and your mental health. Speaking to a licensed mental health professional about these side effects can help you deal with any feelings of depression or anxiety that you may be experiencing.
Your ovaries are reproductive glands located on each side of your pelvis. They’re responsible for making reproductive eggs, also called ova. Your ovaries also serve as your body’s primary source of the hormones estrogen and progesterone. If you have ovaries, you’ve probably experienced pain in them from time to time, typically related to your menstrual cycle. Sometimes, though, ovary pain can be a sign of an underlying condition. Ovarian pain may be felt in the lower abdomen, below the belly button, and pelvis. It can present itself as dull and consistent or as sharp bursts of sensation. While uncomfortable, ovarian pain is not uncommon.
There are many reasons someone may experience ovary pain, including ovarian cysts, ovulation pain, endometriosis, pelvic inflammatory disease or ovarian cancer. The reasons someone would experience ovarian pain may or may not be serious. Treatment will vary depending on what is causing the issue, and by tracking the ovarian pain, a medical professional will better be able to diagnose the cause. Even if the pain is not debilitating, it is important to discuss with a medical professional, preferably a gynecologist, so it can be examined and treated. A gynecologist may perform a complete pelvic exam, including a transvaginal or pelvic ultrasound, radiological tests, a CT scan, and/or a CA-125 blood test to investigate the cause of ovary pain.
Ovarian cysts are fluid-filled masses (unlike ovarian tumors, which are solid), found growing on one or both ovaries. Most ovarian cysts are not harmful and do not trigger symptoms. Symptoms of ovarian cysts: Pelvic or abdominal pain (including ovary pain) Fullness or heaviness in your abdomen Bloating
Pain during ovulation, also known as Mittelschmerz, is experienced when an ovary releases an egg. Generally this happens about fourteen days before the next menstrual period. Symptoms of ovulation pain: Ovary pain usually happens on only one side of the pelvis, and can alternate sides, or stay consistent month-to-month Pain ranges in intensity from dull to sharp
Endometriosis occurs when tissue that looks and acts like endometrial tissue is developed outside the uterus. The endometrial tissue regularly builds each month, and sheds with a person’s menstrual cycle. But for those with endometriosis, the endometrial tissue that is outside of the uterus still reacts to the hormonal fluctuations and results in small bleeding inside the pelvis, outside of the uterus, where the tissue had developed. When it comes specifically to ovarian pain, the monthly breakdown of this tissue can become embedded in the normal ovarian tissue, creating a “blood blister” surrounded by a fibrous cyst, known as an endometrioma.
Pelvic pain (including ovary pain) Pain during intercourse Abnormal or heavy menstrual flow Painful urination during menstrual periods Painful bowel movements during menstrual periods Other gastrointestinal problems
Pelvic inflammatory disease is an infection found in female reproductive organs. It can be brought on by sexually transmitted diseases, such as chlamydia or gonorrhea, or other infections that aren’t not sexually transmitted.
Pain in the lower abdomen (including ovary pain) Fever An unusual discharge with a bad odor from the vagina Pain and/or bleeding during sex Burning sensation during urinating Bleeding between periods
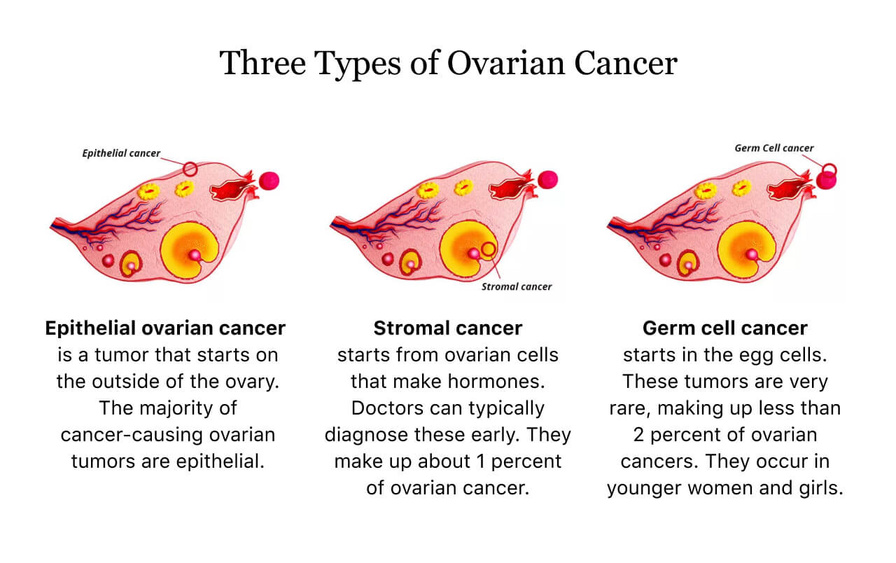
There are several types of ovarian cancers that can lead to ovarian pain, including epithelial ovarian cancer, germ cell ovarian cancer, stromal cell ovarian cancer, and small cell carcinoma (SCCO). While they are all classified as “ovarian” because they concern the ovaries, they range in origin, treatment, and prognosis. As these ovarian cancers develop, tumors grow on one or both ovaries. In some rare cases, early stage ovarian cancers may produce symptoms, but in the majority of patients, these don’t show up until the cancer and tumor growth has advanced, triggering the symptoms.
Ovarian pain that is more severe or more persistent than discomfort associated with a menstrual cycle Bloating Pelvic or abdominal pain (including ovary pain) Difficulty eating or feeling full quickly Urinary symptoms (urgency or frequency) If you are experiencing ovary pain, reach out to a medical professional, preferably a gynecologist, to help determine the cause.