

Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women (1). It is associated with significant morbidity including impaired reproductive health, psychosocial dysfunction, metabolic syndrome, cardiovascular disease, and increased cancer risk (2,3). Controversy continues about the underlying etiopathogenesis, diagnostic criteria, and recommendations for PCOS in adolescents. Recent literature has recognized these deficiencies and evidence based expert recommendations have become more available (4-6). The purpose of this chapter is to offer primary care providers a practical understanding and approach to the diagnosis and treatment of PCOS in adolescents.
Although the pathogenesis is not well understood, PCOS is likely a complex interaction between genetic and environmental factors. Accepted etiologic theories include disordered neuroendocrine gonadotropin secretion, hyperandrogenism, insulin resistance, and hyperinsulinemia or a combination thereof (7). In many, ovarian hyperandrogenism appears to be the primary dysfunction with additional related findings of hyperinsulinism, insulin resistance, elevated luteinizing hormone (LH) and an association of obesity as well. However, it is recognized that there is heterogeneity in this syndrome.

A woman can get PCOS any time after puberty. Most people are diagnosed in their 20s or 30s when they are trying to get pregnant. You may have a higher chance of getting PCOS if you are overweight or have obesity, or if other people in your family have PCOS.
PCOS is very common — up to 15% of women of reproductive age have it.
The most common symptoms of PCOS include:
·Irregular periods: Abnormal menstruation involves missing periods or not having a period at all. It may also involve heavy bleeding during periods.
·Abnormal hair growth: Excess facial hair and heavy hair growth on the arms, chest and abdomen (hirsutism). This affects up to 70% of women with PCOS.
·PCOS can cause acne, especially on the back, chest and face. This acne may continue past the teenage years and may be difficult to treat.
·Obesity: About 80% of women with PCOS are overweight or have obesity, and have trouble losing weight.
·Darkening of the skin: Patches of dark skin, especially in the folds of your neck, armpits, groin (between the legs) and under the breasts. This is known as acanthosis nigricans.
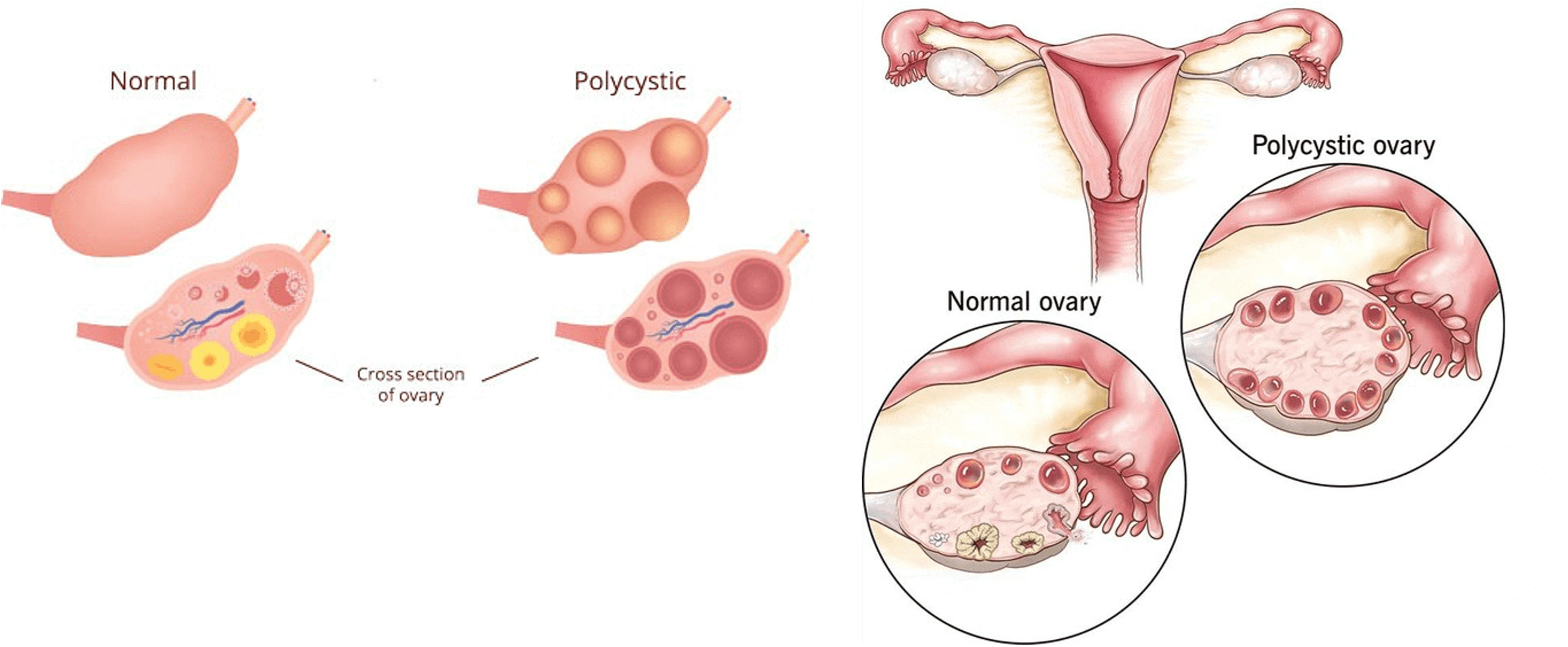
·Cysts: Many women with PCOS have small pockets of fluid in their ovaries.
·Skin tags: Skin tags are little flaps of extra skin. They're often found in the armpits or on the neck in women with PCOS.
·Thinning hair: People with PCOS may lose patches of hair on their heads or start to go bald.
·Infertility: PCOS is the most common cause of female infertility. Decreased frequency or lack of ovulation can result in not being able to conceive.

The exact causes of PCOS is until unknown. There is evidence that genetics play a role. Several other factors also play a role in causing PCOS:
·Higher levels of male hormones called androgens: High androgen levels prevent the ovaries from releasing eggs (ovulation), which causes irregular menstrual cycles. Irregular ovulation can also cause small, fluid-filled sacs to develop in the ovaries. High androgen also causes acne and excess hair growth in women.
·Insulin resistance: Increased insulin levels cause the ovaries to make and release male hormone (androgens). Increased male hormone, in turn, suppress ovulation and contribute to other symptoms of PCOS. Insulin helps your body processes glucose (sugar) and uses it for energy. Insulin resistance means your body doesn't process insulin correctly, leading to high glucose levels in your blood. Not all individuals with insulin resistance have an elevated glucose or diabetes, but insulin resistance can lead to diabetes. Having overweight orobesity can also contribute to insulin resistance. An elevated insulin level, even if your blood glucose is normal, can indicate insulin resistance.
·Low-grade inflammation: People with PCOS tend to have chronic low-grade inflammation. Your healthcare provider can perform blood tests that measure levels of C-reactive protein (CRP) and white blood cells, which can indicate the level of inflammation in your body.

Treatment is dependant on your future condition, If you do not plan to become pregnant, treatments include:
·Hormonal birth control: Options include birth control pills, patches, shots, a vaginal ring or an intrauterine device (IUD). Hormonal birth control helps to regulate your menstrual cycle, improve acne and help with excess hair growth.
·Insulin-sensitizing medicine: Metformin is a drug used to treat diabetes. It works by helping your body process insulin. Once insulin is managed, some people with PCOS see improvements in their menstrual cycles.
·Medications to block androgens: Some drugs can block the effect of androgens. This helps control acne or hair growth caused by PCOS. Talk to your healthcare provider about whether they're right for you.
·Lifestyle changes: Losing weight and eating a healthy diet can have a positive effect on insulin levels.
If you want to become pregnant now or in the future, treatment for PCOS includes:
·Drugs to induce ovulation (releasing an egg): A successful pregnancy begins with ovulation. Certain drugs have been proven to induce ovulation in women with PCOS. The
·medications clomiphene and letrozole are taken orally, while gonadotropins are given by injection.


One of the best ways to cope with PCOS is to lose weight with healthy eating and regular exercise. Even a small amount of weight loss can affect hormone levels and help to regulate your menstrual cycle and ease your symptoms.
If excess hair growth or acne is hurting your confidence, cosmetic treatments or working with a dermatologist might be helpful.
Finally, if you are trying to conceive and have been diagnosed with PCOS, know that you are not alone. Your healthcare provider will work with you to help you get pregnant. Eating healthy and lowering your stress levels can go a long way in helping you manage PCOS.
Endometriosis affects up to 10% of women between the ages of 15 and 44. It most often occurs on or around reproductive organs in the pelvis or abdomen, including:
Fallopian tubes
Ligaments around the uterus (uterosacral ligaments) Lining of the pelvic cavity
Ovaries
Outside surface of the uterus
Space between the uterus and the rectum or bladder
More rarely, it can also grow on and around the:
Bladder
Cervix
Intestines
Rectum
Stomach (abdomen)
Vagina or vulva

Endometrial tissue growing in these areas does not shed during a menstrual cycle like healthy endometrial tissue inside the uterus does. The buildup of abnormal tissue outside the uterus can lead to inflammation, scarring and painful cysts. It can also lead to buildup of fibrous tissues between reproductive organs that causes them to “stick” together.
Endometriosis is a common condition that can interfere with your everyday life. It can cause long-term pain, disruptions to your menstrual cycle and fertility issues. The symptoms of endometriosis are often manageable with treatment
Endometriosis is a condition that most commonly impacts people between the ages of 25 and 40. It can also happen to younger people during their teenage years. Although many people find relief from endometriosis symptoms after menopause, it can still cause discomfort and pain.
The cause of endometriosis is unknown. When you have endometriosis, tissue similar to the lining of your uterus grows in the wrong places. When it develops in places like the outside of your uterus, fallopian tubes, ovaries, intestine and within your pelvic cavity, it can cause painful symptoms. This pain is related to increased inflammation and often fibrosis and adhesions
When endometrial-like tissue grows outside of your uterus, it can cause scar tissue (adhesions). These sections of scar tissue can fuse your organs — creating connections between them that normally wouldn’t be there. This can lead to discomfort and pain.
There are many symptoms connected with endometriosis. The main symptom is pain. This pain can be intense or mild. It can typically be felt in your abdomen, pelvic region and lower back. Although endometriosis is a common condition, not all people will experience symptoms. Sometimes, you can have endometriosis and not know until it’s found during another procedure or investigation of infertility.
People who do experience symptoms of endometriosis may have:
·Very painful menstrual cramps.
·Abdominal pain or back pain during your period or in between periods.
·Pain during sex.
·Heavy bleeding during periods or spotting (light bleeding) between periods.
·Infertility (difficulty becoming pregnant).
·Painful bowel movements.
There’s no connection between the symptoms of endometriosis and the severity of the condition. Some people may have very few patches of endometriosis and still experience severe pain. Other people might have severe endometriosis, but not experience a great deal of pain.
Many people experience pain during periods from endometriosis. This pain is often felt in your abdomen, lower back and pelvic area. Periods can also be heavier than typical, and there can be spotting (light bleeding) between cycles.

Endometriosis has four stages or types. It can be any of the following:
Stage 1: Minimal
In minimal endometriosis, there are small lesions or wounds and shallow endometrial implants on your ovaries. There may also be inflammation in or around your pelvic cavity.
Stage 2: Mild
Mild endometriosis involves light lesions and shallow implants on the ovaries and the pelvic lining.
Stage 3: Moderate
Moderate endometriosis involves many deep implants on your ovaries and pelvic lining. There can also be more lesions.
Stage 4: Severe
The most severe stage of endometriosis involves many deep implants on your pelvic lining and ovaries. There may also be lesions on your fallopian tubes and bowels. There can also be cystsTrusted Source on one or both of your ovaries
The symptoms of endometriosis can be similar to the symptoms of other conditions, such as ovarian cysts and pelvic inflammatory disease. The condition also shares similar symptoms with irritable bowel syndrome (IBS), which can prolong diagnosis.
At the core of treating your pain is getting an accurate diagnosis. It’s important to note that the diagnosis process may vary. In some situations, it can take 4 to 11 years from the onset of symptoms to diagnosis, according to research published in 2019.
Try to be patient with yourself and the process as you work with your healthcare team.
Endometriosis usually develops years after the start of your menstrual cycle. It can be a painful condition.
However, understanding its risk factors can help you determine whether you’re more likely to develop this condition and when you should talk with your docto Women of all ages are at risk for endometriosis. It most commonly affects womenTrusted Source in their 30s and 40s, but symptoms can begin at pubertyTrusted Source.
Talk with your doctor if you have a family member who has endometriosis. You may have a higher risk of developing the disease.
The first step your doctor might recommend is to treat your endometriosis with over-the-counter (OTC) pain medications such as NSAIDs.
If that doesn’t give you the results you need, your next step might be hormone therapy. This includes:
· hormonal contraceptives
· progestin therapy
· aromatase inhibitors
· Gn-RH (gonadotropin-releasing hormone) agonists and antagonists
The final step, if the first steps do not offer you the relief you need, might be surgery
In many cases, your treatment plan will focus primarily on managing your pain and improving fertility issues (if you are planning on a future pregnancy). This can be done through medications and surgery.
Medications are often used to help control the symptoms of endometriosis. These can include pain medications and hormone therapies.
Hormonal options for suppressing endometriosis can include:
· Birth control: There are multiple forms of hormonal suppression options including combination options using estrogen and progesterone or progesterone-only options. These come in multiple forms including oral birth control pills, patch, vaginal ring, birth control shot, Nexplanon implant or IUD. This hormonal treatment often helps people have lighter, less painful periods. These are not options for patients attempting pregnancy.
· Gonadotropin-releasing hormone (GnRH) medications: This medication is actually used to stop the hormones that cause your menstrual cycle. This basically puts your reproductive system on hold as a way to relieve your pain. GnRH medications can be taken as an oral pill (by mouth), a shot or a nasal spray.
· Danazol (Danocrine®): This is another form of hormonal medication that stops the production of the hormones that cause you to have a period. While taking this medication for endometriosis symptoms, you may have the occasional menstrual period, or they might stop entirely.
In some cases, your provider might recommend surgery as a way to confirm and treat endometriosis. There are always risks to a surgical procedure. However, surgery for endometriosis can be an effective way to relieve pain and, in some cases, improve your fertility.
Endometriosis is considered a chronic disease. Many people experience relief from endometriosis pain after surgery, but the symptoms may return within a few years. The severity of your endometriosis could play a part in how quickly — if at all — it comes back after surgery. Your provider might suggest combining a surgical procedure with medications for the best outcome. Your provider may recommend pelvic floor physical therapy with or without medications for central nerve pain.
Surgical options to treat endometriosis include:
· Laparoscopy: In this procedure, your surgeon will make a very small cut in your abdomen (< 1 centimeter) and insert a thin tube-like tool called a laparoscope into your body. This tool can be used to see inside your body and identify endometriosis with a high-definition camera. Additional 5- millimeter instruments can then be used to excise and remove lesions.
· Hysterectomy: In severe cases, your surgeon may suggest removing your uterus based on the amount of endometriosis and scar tissue present, if you have other uterine conditions like adenomyosis and your desire for future fertility. If you have a hysterectomy, areas of endometriosis should still be excised to optimize your pain relief.
